Expanding HIV testing provision and uptake through the use of tents
|
Mangochi is a district in Southeastern Malawi with a high HIV prevalence of 10.1%[1]. Baylor College of Medicine Children’s Foundation Malawi (Baylor) through the Tingathe program is supporting Malawi’s Ministry of Health to meet the ambitious 90-90-90 goals for HIV status knowledge, treatment and viral suppression in the district.
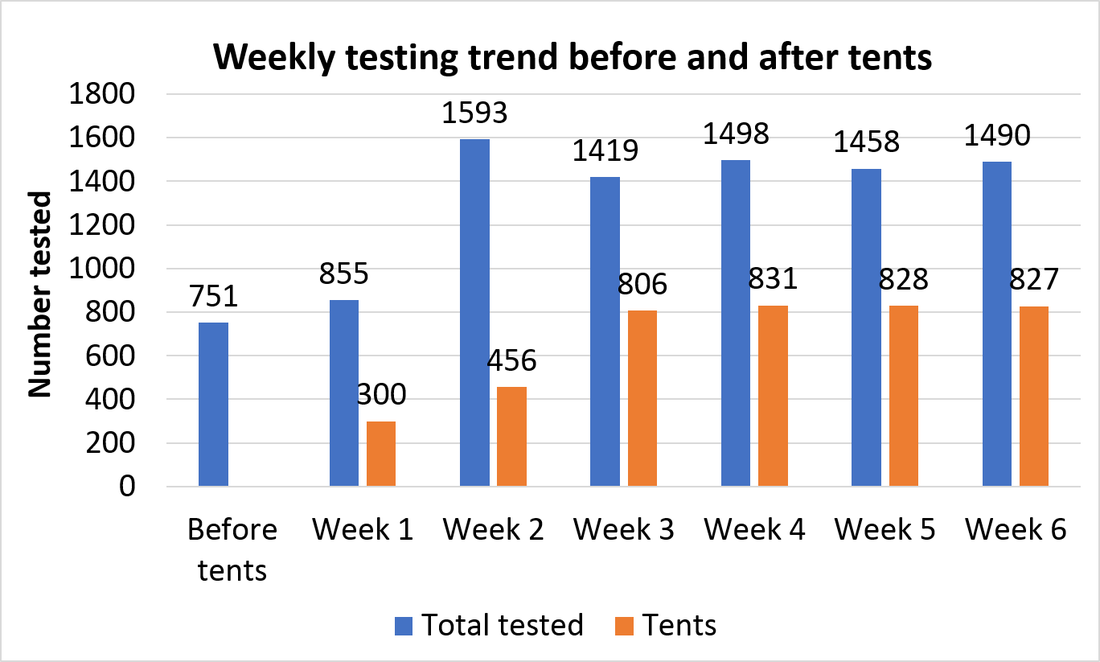
Baylor takes a comprehensive approach to HIV case identification, striving to offer HIV testing services to every client accessing medical care at a health facility, as well as their families and communities. This approach includes screening and providing testing in multiple settings: inpatient and outpatient provider-initiated testing and counselling, weekend and evening testing, intensified index case testing, targeted community testing, and outreach testing. A review of program performance revealed that a lack of space was a key barrier to success, despite multiple opportunities for offering testing to clients. The provision of quality HIV testing services necessitates a clean, well-equipped, confidential space, but gaps identified at health facilities in the district included poorly located testing sites which undermined access (such as clients having to walk across the facility to access testing rooms), inadequate number of testing rooms, and poor condition of existing testing rooms (such as poor lighting and a lack of confidentiality). To address these barriers, the Tingathe program embarked upon a process of mounting tents at selected facilities as a rapid solution to provide quality testing services. At Mangochi District Hospital (MDH), the provision of three tents resulted in a significant increase in the number of people accessing HIV testing services. Notably, testing coverage in the tents surpassed testing provided in the facility by week three. The approach has nearly doubled the number of people tested prior to implementation of this approach, from an average of 751 tested before the tents to an average of 1,386 tested in the six weeks after the tents were mounted. The tents were used to test people attending departments that had limited access to testing points before but served higher-risk patients, including sexually-transmitted infection, outpatient and family planning clinics. The success of this approach demonstrates that a simple solution – provision of testing tents – can have a significant impact in terms of improving access and testing conditions such as privacy, consequently increasing HIV testing service uptake and case identification. [1] Malawi DHS 2015; overall HIV prevalence in Malawi is 8.8% among those aged 15-49 years |