A two-year-old enrolled into care courtesy of health talks
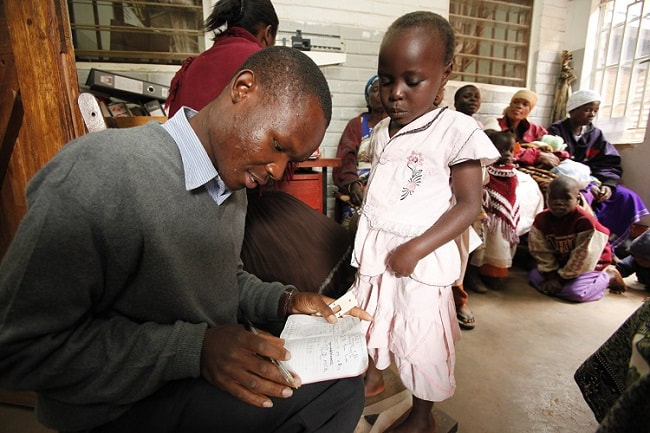
Health talks are given by community health workers in the outpatient department (OPD) on a daily basis to encourage clients to go for an HIV test, or return to care.
In September 2020, a 40-year-old woman attended OPD at Machinga District Hospital (MDH) with her two-year-old grandson. She has been looking after her grandson for four months since his mother had married. The grandmother had attended the hospital a number of times previously as her grandson had been unwell for some time. He had recurrent skin rashes and malaria a number of times. The child’s persistent ill health was of great concern to the grandmother.
On this clinic day, she had come in early with the hope of being seen quickly so that she could go back home. While she was waiting to see the clinician, Memory, a CHW from BCM, started to give a health talk on the benefits getting an HIV test. The child’s grandmother sat in the crowd and listened attentively. At the end of the talk, she had many questions. She wondered if her grandson could be HIV positive. She wondered if she could ask for the child to be tested, even though she was not the mother. She stood up and asked for assistance. She received counselling and the child was tested. He was found to be positive and started on LPV/r granules immediately.
The grandmother and child were referred to the psychosocial counselor. The grandmother appeared distressed and extremely sad for the child, but was pleased that she had identified a reason for her grandson’s ill health and that she was able to have hope that he might become healthy again. The grandmother felt confident that starting on ART would lead to improved health and resolving persistent illness. The child’s mother would be encouraged to come for testing.
In September 2020, a 40-year-old woman attended OPD at Machinga District Hospital (MDH) with her two-year-old grandson. She has been looking after her grandson for four months since his mother had married. The grandmother had attended the hospital a number of times previously as her grandson had been unwell for some time. He had recurrent skin rashes and malaria a number of times. The child’s persistent ill health was of great concern to the grandmother.
On this clinic day, she had come in early with the hope of being seen quickly so that she could go back home. While she was waiting to see the clinician, Memory, a CHW from BCM, started to give a health talk on the benefits getting an HIV test. The child’s grandmother sat in the crowd and listened attentively. At the end of the talk, she had many questions. She wondered if her grandson could be HIV positive. She wondered if she could ask for the child to be tested, even though she was not the mother. She stood up and asked for assistance. She received counselling and the child was tested. He was found to be positive and started on LPV/r granules immediately.
The grandmother and child were referred to the psychosocial counselor. The grandmother appeared distressed and extremely sad for the child, but was pleased that she had identified a reason for her grandson’s ill health and that she was able to have hope that he might become healthy again. The grandmother felt confident that starting on ART would lead to improved health and resolving persistent illness. The child’s mother would be encouraged to come for testing.
